3. Preparing for a Rigid Bronchoscopy
Pre-Procedural Assessments and Patient Selection
Before undergoing a rigid bronchoscopy, patients undergo a comprehensive evaluation to assess their suitability for the procedure and to plan the intervention carefully. This assessment typically includes a detailed medical history, physical examination, and review of previous imaging studies, such as X-rays or CT scans, to understand the anatomy and pathology of the airways. Pulmonary function tests and blood work may also be conducted to evaluate the patient’s respiratory status and overall health. Patient selection is based on the indication for bronchoscopy, the potential risks and benefits, and the patient’s ability to tolerate the procedure under general anesthesia.
Patient Preparation: What to Expect Before the Procedure
Patients are usually instructed to fast for a certain period before the procedure to minimize the risk of aspiration during anesthesia. Pre-operative medications may be administered to help with relaxation and to reduce secretions. The healthcare team will also discuss what to expect during and after the procedure, including potential risks and the recovery process. Informed consent is obtained, ensuring that the patient or their legal guardian understands the procedure’s purpose, benefits, and risks.
The Role of the Multidisciplinary Team
A multidisciplinary team approach is crucial for the successful outcome of a rigid bronchoscopy. This team typically includes a thoracic surgeon or pulmonologist with expertise in rigid bronchoscopy, an anesthesiologist experienced in airway management, nursing staff, and, when necessary, other specialists such as interventional radiologists or oncologists. The team works together to plan the procedure, manage any complications, and provide comprehensive post-procedural care, ensuring the best possible outcomes for the patient.
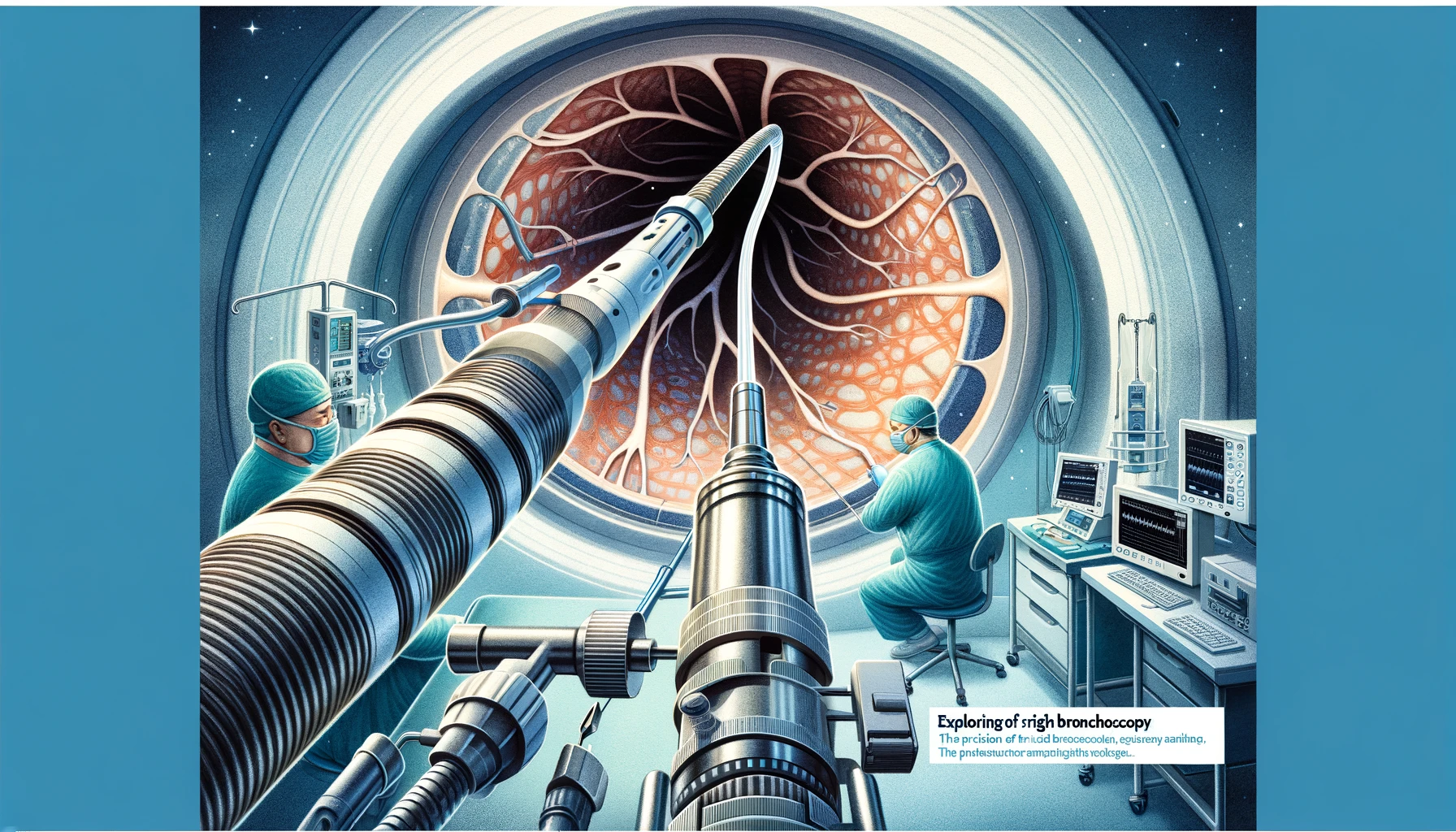
The Rigid Bronchoscopy Procedure
Step-by-Step Guide to the Procedure
- Anesthesia and Airway Access: The procedure begins with the administration of general anesthesia and the establishment of a secure airway, often through intubation.
- Insertion of the Bronchoscope: Once the patient is sedated, the rigid bronchoscope is carefully inserted through the mouth (or occasionally the nose) and advanced towards the trachea and bronchi.
- Inspection and Intervention: The surgeon inspects the airway, identifying any abnormalities. Therapeutic interventions, such as biopsy, foreign body removal, or tumor debulking, are performed as needed.
- Completion: After the necessary interventions are completed, the bronchoscope is slowly withdrawn, ensuring the airway remains clear.
- Recovery: The patient is closely monitored as they recover from anesthesia and is typically observed for several hours post-procedure for any complications.
Anesthetic Considerations
General anesthesia with muscle relaxation is typically required for rigid bronchoscopy to ensure patient comfort and immobilization, as well as to facilitate control of the airway. Close coordination between the bronchoscopist and the anesthesiologist is essential to manage the airway and ensure adequate ventilation and oxygenation throughout the procedure. Special techniques, such as jet ventilation, may be used to maintain oxygenation while providing the surgeon with enough space to work within the airway.
Tools and Techniques Utilized During Rigid Bronchoscopy
The rigid bronchoscope itself is a straight, hollow metal tube with a light source and a connection for oxygen supply. Various instruments can be passed through the bronchoscope, including forceps for biopsy or foreign body removal, brushes for cytology samples, and lasers or other devices for cutting or cauterizing tissue. Advanced techniques such as cryotherapy, electrocautery, and placement of stents to keep the airway open may also be employed. The choice of tools and techniques depends on the specific goals of the procedure, highlighting the versatility of rigid bronchoscopy in diagnosing and treating a wide range of airway conditions.