Botulism (clostridium botulinum)
Overview of Botulism
Botulism is a rare but severe condition caused by toxins produced by the bacterium Clostridium botulinum. If not treated promptly and effectively, it can lead to severe neurological symptoms, including muscle weakness, paralysis, and even death. It comes in various forms, primarily foodborne, wound, infant, and iatrogenic, each associated with different sources of exposure to the toxin. Due to its severity, understanding it is crucial for timely diagnosis and management.
Importance of Awareness and Early Detection
Awareness and early detection of Botulism are vital for several reasons. First, its symptoms, especially in its early stages, can be easily confused with those of other conditions, leading to delays in diagnosis and treatment. Second, because it can progress rapidly, leading to respiratory failure and other severe complications, early intervention can be life-saving. Educating the public and healthcare providers about its signs and symptoms and potential sources is crucial in preventing outbreaks and ensuring prompt treatment.
Understanding Types of Botulism
What is Botulism?
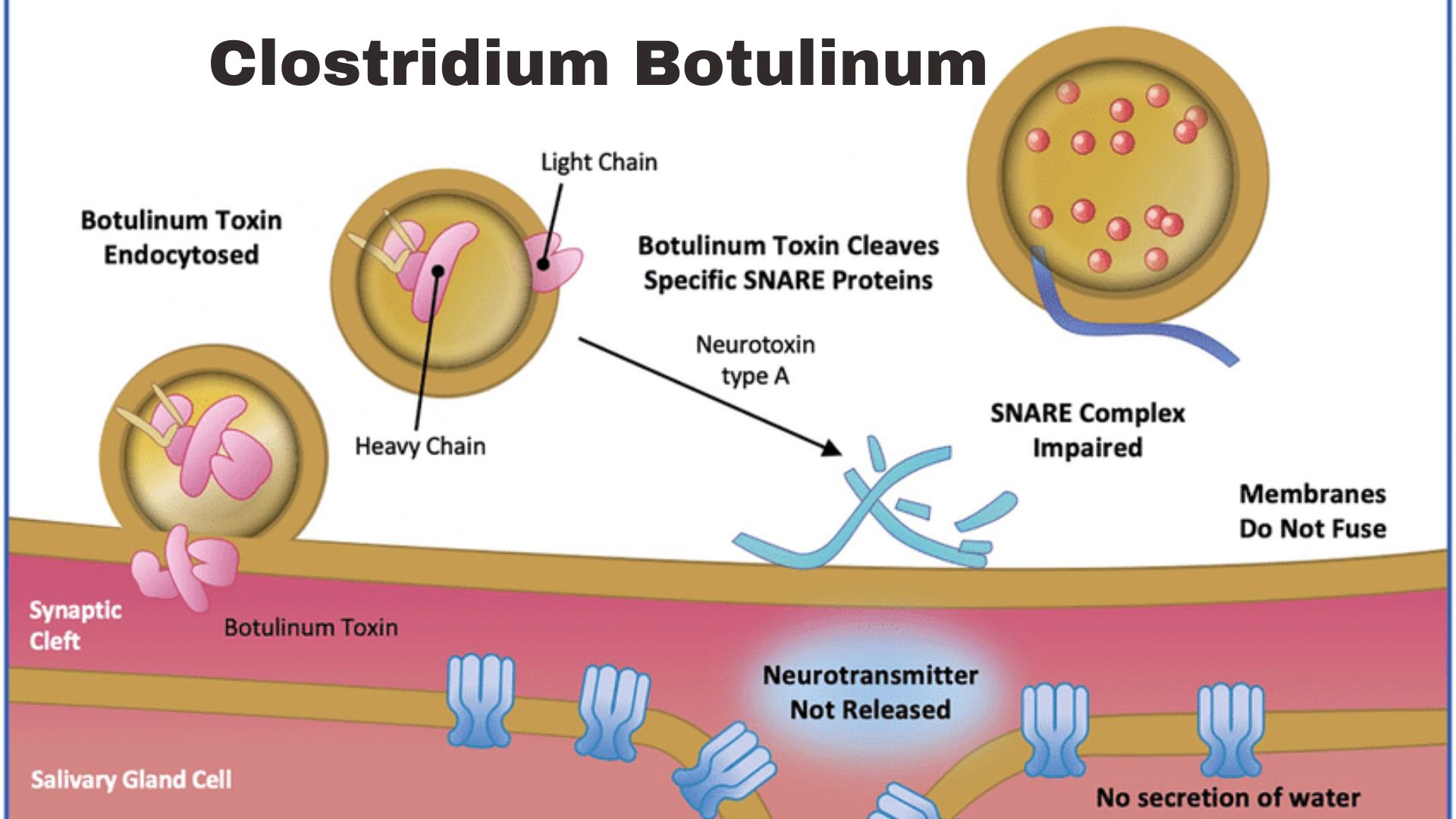
Botulism is a potentially fatal illness caused by the neurotoxins produced by the Clostridium botulinum bacteria. These toxins are among the most potent known to science and exert their effect by blocking nerve functions, leading to respiratory and muscular paralysis. The disease does not spread from person to person but is acquired from the environment.
Types of Botulism
It can manifest in several forms with distinct causes and transmission routes. Understanding these types is crucial for effective prevention and treatment.
Foodborne Botulism
Foodborne (B) is caused by consuming foods contaminated with botulinum toxin. It is often associated with improperly canned, preserved, or fermented foods at home. Symptoms typically arise within 12 to 36 hours after ingestion of the toxin-laden food.
Infant Botulism
Infant (B) occurs when infants ingest Clostridium botulinum spores, which can grow and produce toxins in the intestines. Familiar sources include honey and environmental dust containing the spores. It is the most common form of it in the United States.
Wound Botulism
Wound (B) results from the contamination of a wound by Clostridium botulinum spores, where they can germinate and produce toxins. It is often associated with injection drug use, especially when using black-tar heroin.
Iatrogenic Botulism
Iatrogenic (B) can occur following the administration of excessive amounts of botulinum toxin for cosmetic or therapeutic purposes. Although rare, it highlights the importance of professional expertise and moderation in botulinum toxin.
Causes and Transmission
The underlying cause is exposure to the botulinum toxin produced by the bacterium Clostridium botulinum. Transmission varies by type but generally involves either the ingestion of the toxin (foodborne and infant (B)), direct bacterial infection of a wound (B), or accidental overdose of botulinum toxin (iatrogenic (B)). Understanding these pathways is fundamental to preventing and mitigating the disease’s impact on affected individuals.
- Causes:
- Genetic factors: Certain conditions are inherited or have a predisposition based on family history.
- Environmental exposure: Contact with pollutants, chemicals, or other hazardous materials can lead to diseases.
- Transmission:
- Person-to-person: Diseases can spread through physical contact, respiratory droplets, or bodily fluids.
- Vector-borne: Some diseases are transmitted through the bites of infected insects or animals.
FAQs on Botulism
Q1: What is botulism?
It is a rare but severe illness caused by botulinum toxin. It can lead to paralysis, breathing difficulties, and potentially death. It typically results from consuming contaminated food, exposure to infected wounds, or, in infants, ingesting spores found in soil or honey.
Q2: How can botulism be prevented?
Prevention includes safe food handling and preparation, such as proper canning, cooking, and storing foods; avoiding giving honey to infants under one year; and seeking prompt medical care for infected wounds.
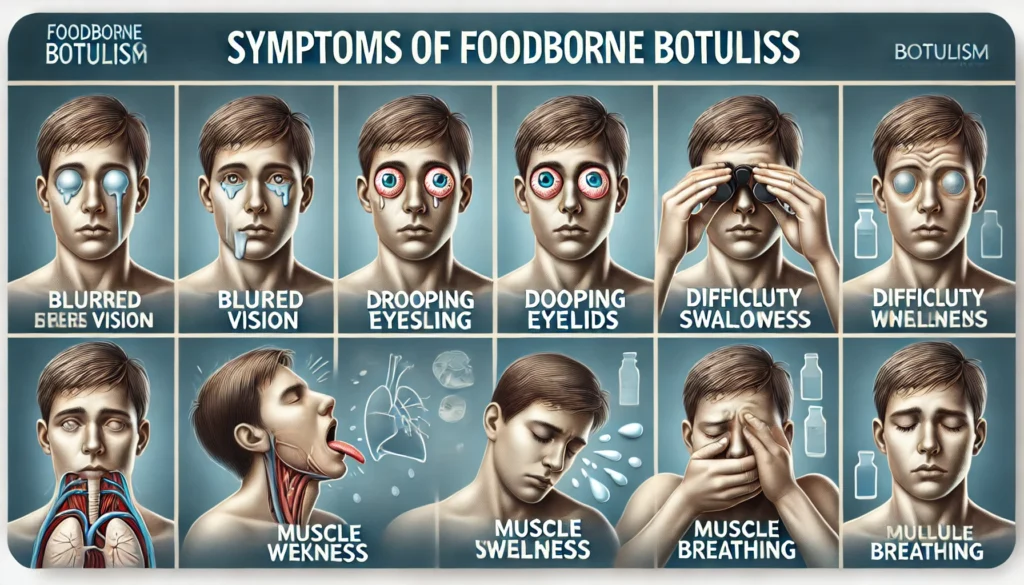
Q3: What are the symptoms of Botulism?
Symptoms often begin with weakness, blurred vision, tiredness, and trouble speaking or swallowing. They may progress to muscle weakness, difficulty breathing, and paralysis.
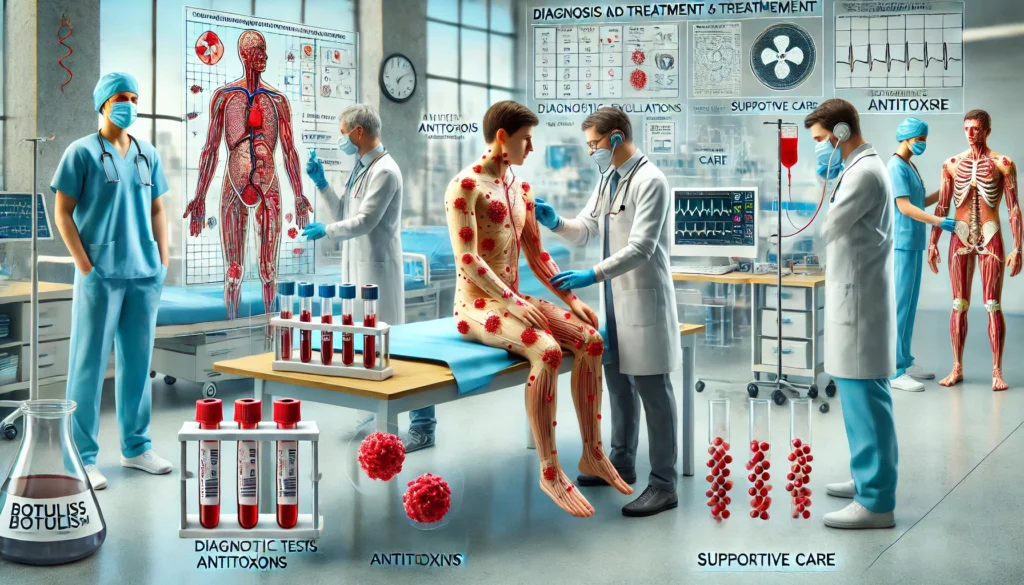
Q4: How is Botulism treated?
Treatment may involve administering antitoxins to neutralize the toxin and providing supportive care, such as mechanical ventilation for breathing, wound antibiotics, and long-term rehabilitation therapy to recover muscle strength.
Q5: Is Botulism contagious?
No, they are not contagious and cannot be spread from person to person. It results from ingesting the toxin or, in the case of wound them, having an infected wound.