ETIS Mutation and Wiskott-Aldrich syndrome
Overview of ETIS
Eczema Thrombocytopenia Immunodeficiency Syndrome (ETIS) is a rare, complex condition characterized by a triad of symptoms: eczema, thrombocytopenia, and also immune deficiency foundation. Eczema, a condition causing inflamed, itchy, and red skin, is often the most visible of these symptoms. Thrombocytopenia, the reduction in the number of platelets that are crucial for blood clotting, can lead to excessive bleeding and bruising. Immune deficiency refers to the body’s impaired ability to fight infections, making individuals more susceptible to illnesses. The convergence of these three components forms a syndrome that poses significant challenges in diagnosis and management due to its varied manifestations and the overlap with other conditions.
Importance of Understanding ETIS
Understanding Eczema Thrombocytopenia Immunodeficiency Syndrome is vital for several reasons. First, it can facilitate early and accurate diagnosis, which is crucial for managing symptoms and improving quality of life. Knowledge about the syndrome can lead to better-targeted treatments that address all aspects of the condition rather than focusing on individual symptoms. Awareness among healthcare professionals and the public can also enhance support for affected individuals, providing them with the necessary resources and community understanding. Finally, comprehension of Eczema Thrombocytopenia Immunodeficiency Syndrome can spur research into more effective treatments and potentially a cure, highlighting the importance of studying this rare syndrome.
Rare Disease ETI syndrome
Eczema Thrombocytopenia Immunodeficiency Syndrome
Eczema Thrombocytopenia Immunodeficiency Syndrome is a rare condition that manifests through a combination of eczema, low platelet count, and weakened immune system. The syndrome’s rarity and the commonality of its components with other diseases make ETIS particularly challenging to diagnose. Patients with Eczema Thrombocytopenia Immunodeficiency Syndrome often experience a range of symptoms, from mild to severe, impacting their skin, blood, and immune system’s ability to fight infections.
The Connection Between Eczema, Thrombocytopenia, and Immunodeficiency
The interplay between eczema, thrombocytopenia, and immunodeficiency in ETIS is complex and not fully understood. These conditions can exacerbate each other, creating a cycle that complicates treatment and management. For example, the skin barrier disruption in eczema can increase the risk of infection, which is particularly problematic given the immunodeficiency component of ETIS. Similarly, thrombocytopenia can lead to issues with wound healing, further increasing infection risk. This intricate relationship underscores the need for an integrated treatment approach that addresses all three aspects of the syndrome.
Causes and Risk Factors
The exact causes of ETIS are currently unknown, and ongoing research aims to uncover the genetic, environmental, and immunological factors that may contribute to its development. Syndrome protein deficiency is also helpful. Some evidence suggests a genetic predisposition to the syndrome, with certain genetic disorders being investigated for their roles in affecting immune system function and skin health. Environmental factors, including exposure to certain infections or allergens, may also play a role in triggering or exacerbating the condition. Understanding these causes and risk factors is crucial for developing preventive strategies and targeted therapies for ETIS.
Eczema Thrombocytopenia Immunodeficiency Syndrome is a multifaceted condition that requires a comprehensive understanding to ensure effective management and support for those affected. Through ongoing research and increased awareness, there is hope for more effective treatments and a better quality of life for individuals with ETIS.
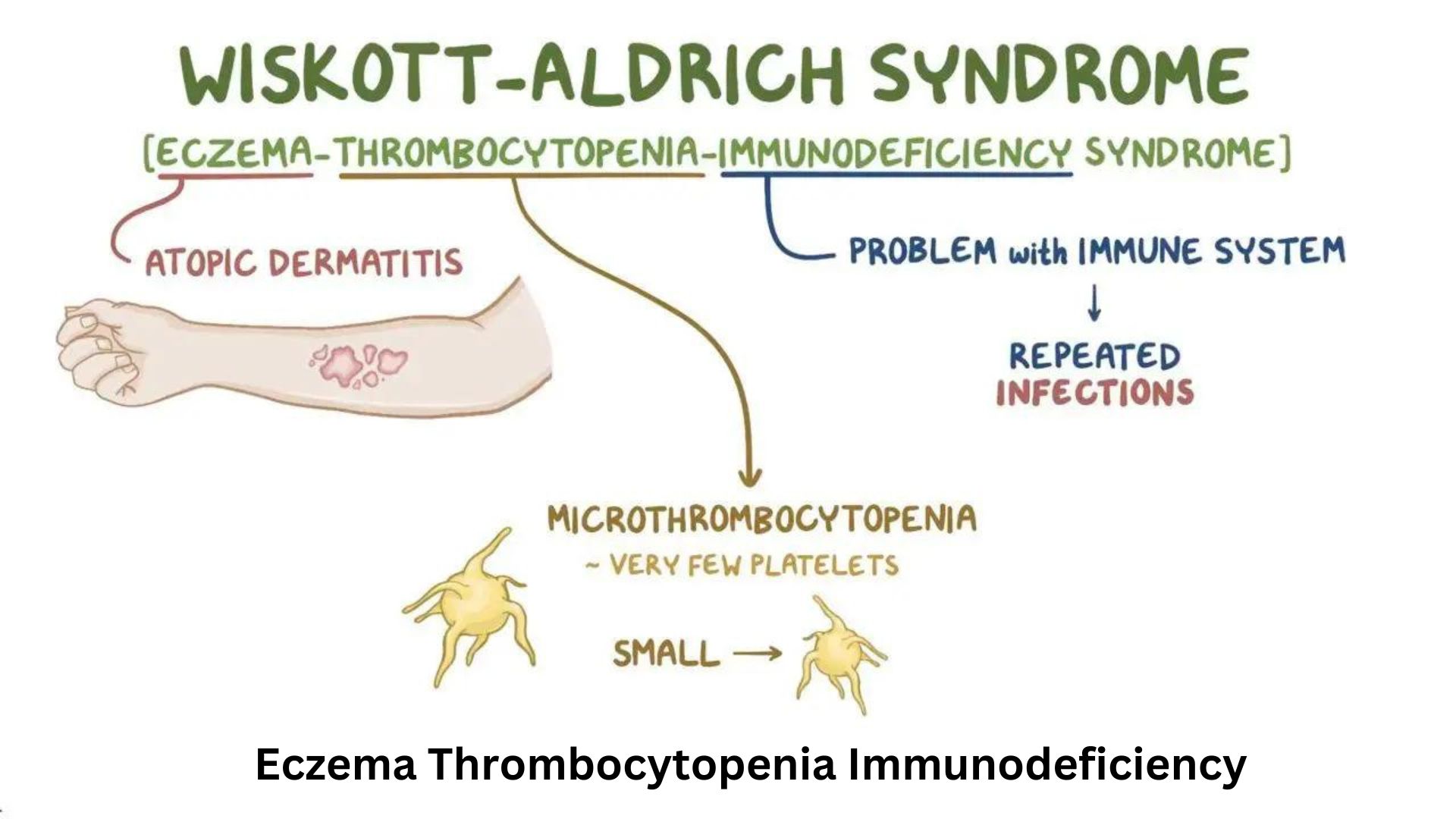
Wiskott-Aldrich Syndrome (WAS) is a rare genetic disorder characterized by a triad of symptoms: eczema, recurrent infections due to immunodeficiency, and a low platelet count (thrombocytopenia), which leads to bleeding. It primarily affects males due to its X-linked recessive inheritance pattern. X-linked thrombocytopenia is also affected Understanding the symptoms and the process of diagnosing WAS is crucial for managing the condition effectively.
Symptoms of Wiskott-Aldrich Syndrome
- Eczema: Patients often present with eczema, a skin condition that causes itchy, inflamed, and red skin patches.
- Thrombocytopenia: A low platelet count leads to easy bruising, frequent nosebleeds, blood in the urine or stool, and prolonged bleeding from cuts. The small size of platelets is a characteristic feature.
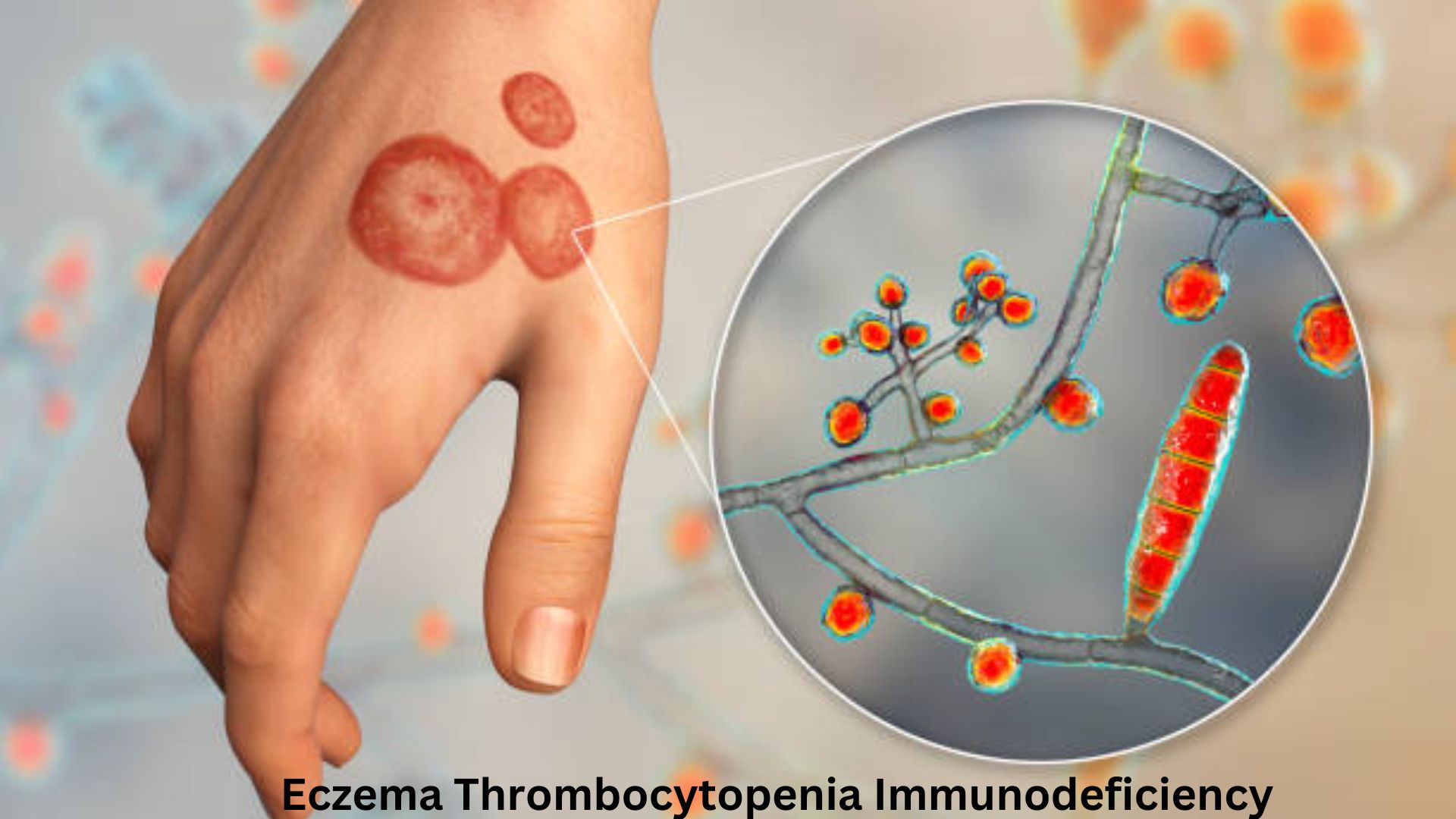
- Immunodeficiency: WAS patients are more susceptible to infections due to a weakened immune system. These infections can be bacterial, viral, or fungal and are often more severe and recurrent.
- Autoimmune Disorders: Some individuals may develop autoimmune diseases where the immune system attacks the body’s b cells and tissues. If autoimmunity does not work then our body starts to lose function.
- Increased Risk of Cancers: A higher risk of developing lymphoma and other cancers exists. if any incidence occurs through donor transplantation or cell transplantation then it may be lead to hemolytic anemia or gene mutation.
Diagnosis of Wiskott-Aldrich Syndrome
1. Clinical Evaluation
- Diagnosis begins with a thorough clinical evaluation, including a detailed patient history and physical examination, focusing on the triad of symptoms.
2. Blood Tests
- Complete Blood Count (CBC): To check for low platelet count and small platelet size.
- Immunoglobulin Levels: To assess the immune system’s functioning, which can be abnormal in WAS.
- Lymphocyte Panel: To evaluate the number and function of white blood cells involved in the immune response.
3. Genetic Testing
- Confirmatory genetic testing for mutations in the WAS gene (located on the X chromosome) is essential for a definitive diagnosis. This test can identify the specific error causing the disorder.
4. Immunological Tests
- Assessing the immune system’s ability to respond to infections effectively, including specific antibody response tests after vaccination or exposure to pathogens.
Differential Diagnosis
Eczema Thrombocytopenia Immunodeficiency Syndrome must be differentiated from other conditions with similar symptoms, such as immune thrombocytopenic purpura (ITP), severe combined immunodeficiency (SCID), and other primary immunodeficiency disorders. The unique combination of symptoms, along with genetic testing, helps distinguish WAS from these conditions.
Signs and symptoms of Eczema Thrombocytopenia Immunodeficiency Syndrome
Identifying Symptoms of ETIS
The symptoms of Eczema Thrombocytopenia Immunodeficiency Syndrome (ETIS) can vary widely among individuals but generally encompass issues related to the skin, blood, and immune system. Eczema typically presents as dry, itchy, and inflamed patches (wasps) of skin, which can lead to scratching and subsequent infections. Thrombocytopenia manifests through symptoms such as easy bruising, prolonged bleeding from cuts, petechiae (small red or purple spots due to bleeding under the skin), and in severe cases, bleeding in the gums, nose, or gastrointestinal tract. Immunodeficiency in ETIS patients leads to an increased susceptibility to infections, including those that are common (like colds) and those that are more serious or opportunistic. Hematopoietic stem cells have a higher performance as compared to hematopoietic cells.
Diagnostic Tests and Criteria for ETIS
Diagnosing Eczema Thrombocytopenia Immunodeficiency Syndrome involves a combination of clinical evaluation and laboratory tests. The diagnosis is primarily based on the presence of the syndrome’s three hallmark symptoms. However, given the rarity and complexity of ETIS, a definitive diagnosis often requires:
- Complete Blood Count (CBC) with differential to assess platelet levels.
- Skin biopsy from an eczematous lesion to confirm the presence and characteristics of eczema.
- Immunoglobulin levels and specific antibody tests to evaluate immune function.
- Genetic testing may be considered to identify specific errors that could be associated with ETIS, though the genetic basis of the syndrome is not fully understood.
Differential Diagnosis – Distinguishing ETIS from Other Conditions
ETIS must be differentiated from other conditions that can present with similar symptoms, such as Wescott-Aldrich syndrome, severe combined immunodeficiency (SCID), and other primary immunodeficiency disorders. A detailed patient history, thorough clinical examination, and targeted laboratory tests are crucial for distinguishing Eczema Thrombocytopenia Immunodeficiency Syndrome from these other conditions, allowing for accurate diagnosis and appropriate management.
Treatment options and Management
Treatment Options for ETIS
The treatment of ETIS is multidisciplinary and aims to manage symptoms and prevent complications. Stem cells are also helpful for preventing the System. There is no cure for Eczema Thrombocytopenia Immunodeficiency Syndrome, so treatment focuses on managing each component of the syndrome:
- Immunoglobulin Replacement Therapy can be used to boost the immune system in patients with significant immunodeficiency.
- Corticosteroids and other immunosuppressive agents may be prescribed to control inflammation and manage eczema and autoimmune manifestations.
- Platelet Transfusion may be necessary in cases of severe thrombocytopenia, especially if there is significant bleeding. if cell function not perform estimated incidence in the right way. it may lead to bloody diarrhea
Managing Eczema in ETIS
Management of eczema in Eczema Thrombocytopenia Immunodeficiency Syndrome patients involves regular skincare routines, including the use of moisturizers to maintain skin hydration and barrier creams to protect the skin. Topical corticosteroids or calcineurin inhibitors may be used to reduce inflammation and itching. Avoidance of known triggers, such as certain foods, allergens, or irritants, is also important.
Addressing Thrombocytopenia and Immunodeficiency
Thrombocytopenia may require interventions such as platelet transfusions in acute bleeding situations or splenectomy in refractory cases. Immunodeficiency is managed through vigilant infection prevention, prompt treatment of infections, and possibly prophylactic antibiotics. Immunoglobulin replacement therapy can significantly improve the quality of life by reducing the frequency and severity of infections.
Lifestyle and Home Care Recommendations
Lifestyle modifications and home care play a crucial role in managing Eczema Thrombocytopenia Immunodeficiency Syndrome:
- Infection Prevention: Good hygiene practices and avoiding exposure to infectious agents are critical.
- Skin Care Routine: Regular and gentle skin care can help manage eczema symptoms and prevent skin infections.
- Diet and Nutrition: A balanced diet that supports immune function and overall health is recommended.
- Stress Management: Stress can exacerbate eczema; thus, stress-reducing activities and adequate sleep are important.
By integrating medical treatments with lifestyle and home care strategies, individuals with ETIS can manage their symptoms more effectively and improve their quality of life. Collaboration between patients, families, and a multidisciplinary healthcare team is essential for optimal management of Eczema Thrombocytopenia Immunodeficiency Syndrome. Also, visit my other post, Automated Dispensing Cabinets.
Living with Eczema Thrombocytopenia Immunodeficiency Syndrome
Daily Life and Coping Strategies
Living with Eczema Thrombocytopenia Immunodeficiency Syndrome (ETIS) involves navigating a variety of challenges, from managing symptoms to coping with the emotional and psychological impacts of the condition. Developing effective coping strategies is crucial. This may include establishing a routine for skin care, medication, and monitoring for infections, as well as finding ways to manage stress and anxiety. Building a strong support network, including family, friends, and healthcare professionals, can provide invaluable emotional support and practical assistance. Education about ETIS helps patients and their caregivers advocate for appropriate care and accommodations in schools, workplaces, and social settings.
Nutrition and Exercise
A balanced diet that supports immune health and overall well-being is important for individuals with ETIS. While there’s no specific diet for ETIS, consuming a variety of fruits, vegetables, whole grains, and lean proteins can help maintain overall health and potentially improve the body’s ability to fight infections. Regular, moderate exercise is encouraged as it can boost mood, improve cardiovascular health, and strengthen the immune system. However, activities should be chosen carefully to avoid injury, especially in individuals with severe thrombocytopenia.
Support and Resources for Patients and Families
Finding comprehensive support and reliable resources can make a significant difference in managing ETIS. Support groups, either online or in-person, can offer a platform to share experiences and coping strategies. Patient advocacy organizations and specialized clinics for rare disorders can provide educational materials, guidance on treatment options, and connections to clinical trials. Psychological support through counseling or therapy can also be beneficial in addressing the emotional and mental health challenges associated with chronic illness.
Research and Future Directions Current Research on ETIS
Research on ETIS is ongoing and aims to better understand the underlying mechanisms of the syndrome, develop more effective treatments, and improve patient outcomes. Current studies may focus on the genetic factors that contribute to the condition, the immune system’s role in the syndrome, and how the environment affects individuals with Eczema Thrombocytopenia Immunodeficiency Syndrome. Advances in genomics and immunology are providing new insights into the syndrome, potentially leading to targeted therapies.
- Genetic Studies: Researchers are exploring the genetic basis of ETIS, focusing on identifying specific mutations that may contribute to the syndrome.
- Immunological Research: Efforts are underway to understand the immune system abnormalities in ETIS, aiming to improve immunodeficiency management.
- Skin Barrier Function: Studies investigate the skin’s barrier function in ETIS to develop better treatments for eczema associated with the syndrome.
- Treatment Trials: Clinical trials are testing new medications and therapies to manage symptoms of ETIS more effectively.
- Quality of Life Research: Investigations are also focusing on the impact of Eczema Thrombocytopenia Immunodeficiency Syndrome on quality of life and how best to support patients and families.
Potential Future Treatments and Therapies
The future of Eczema Thrombocytopenia Immunodeficiency Syndrome treatment looks promising as research advances. Gene therapy, for example, offers the potential to correct underlying genetic abnormalities that contribute to the syndrome. Advances in immunotherapy could provide more effective ways to manage the immunodeficiency aspect of ETIS, reducing the risk of infections and improving quality of life. Personalized medicine, based on the specific genetic and immunologic profile of each patient, may also play a role in future treatments.
The Importance of Clinical Trials
Clinical trials are crucial for the development of new treatments and therapies for Eczema Thrombocytopenia Immunodeficiency Syndrome. They offer patients the opportunity to access cutting-edge treatments and play a vital role in advancing medical knowledge about the syndrome. Participation in clinical trials also helps researchers better understand the effectiveness and safety of potential new treatments, paving the way for advances in care. Patients and families are encouraged to consider clinical trials as a treatment option, contributing to the progress toward better outcomes for those with ETIS.
Living with ETIS presents unique challenges, but with the right support, management strategies, and advancements in research, patients can lead fulfilling lives. The ongoing dedication of the medical community to understanding and treating ETIS holds promise for future breakthroughs that could significantly improve the lives of those affected by this complex syndrome.
(FAQs)
What is the prognosis for someone with ETIS?
The prognosis for Eczema Thrombocytopenia Immunodeficiency Syndrome varies depending on the severity of symptoms and how well the condition is managed.
Can ETIS be cured or only managed?
Currently, there is no cure for ETIS, and the focus is on managing symptoms and preventing complications. Treatment strategies are tailored to the individual’s specific symptoms and may include medications, therapy, and lifestyle adjustments.
How does ETIS affect children differently from adults?
Children with ETIS may face additional challenges, including growth and development issues, and may require special considerations in their treatment and care. Early intervention and support are crucial to help manage the condition and support normal development.
Are there genetic components to ETIS?
While the exact cause of ETIS is not fully understood, researchers believe that genetic factors may play a role in its development. Ongoing research aims to identify specific genetic mutations that could be linked to Eczema Thrombocytopenia Immunodeficiency Syndrome.
How can families of individuals with ETIS find support?
Families can find support through various channels, including patient advocacy organizations, online support groups, and healthcare professionals specializing in rare diseases. These resources can provide valuable information, emotional support, and connections to other families navigating similar challenges.
Conclusion
Eczema Thrombocytopenia primary Immunodeficiency Syndrome (ETIS) represents a complex, multifaceted condition that, while challenging, can be managed with a comprehensive approach to treatment and support. Advances in medical research continue to shed light on the underlying mechanisms of ETIS, offering hope for more effective treatments and potentially a cure in the future. For individuals living with Eczema Thrombocytopenia Immunodeficiency Syndrome and their families, accessing reliable information, medical care, and supportive communities is essential for navigating the challenges of the syndrome. With ongoing research, increased awareness, and a supportive network, the outlook for those affected by Eczema Thrombocytopenia is continually improving, promising a better quality of life and brighter prospects ahead.
1 thought on “Eczema Thrombocytopenia Immunodeficiency Syndrome”