Cleft Lip and Cleft Palate Repair
Understanding Cleft Palate
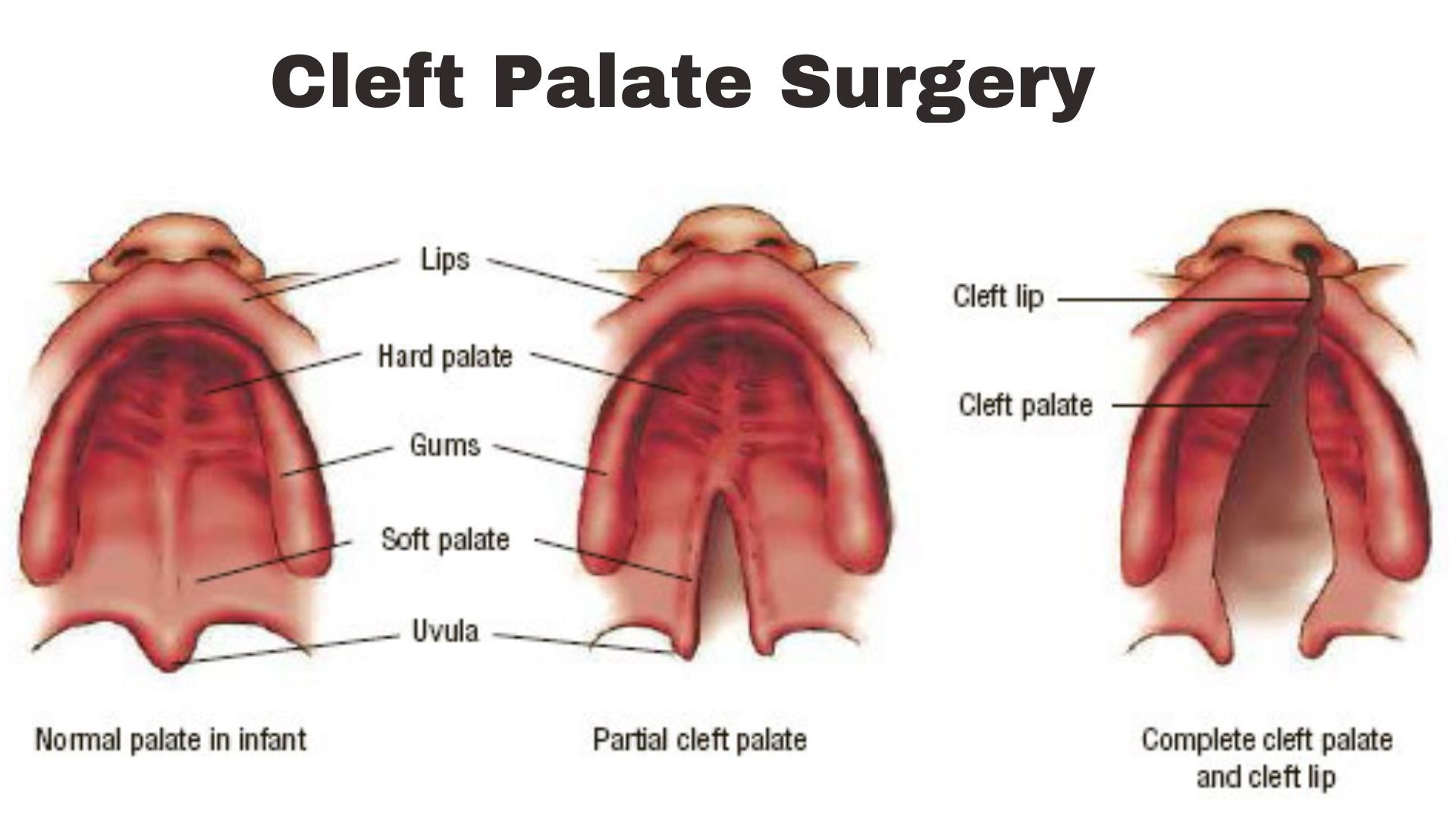
Cleft palate surgery is a congenital deformity that occurs when the roof of the mouth, known as the palate, fails to form during early pregnancy fully. This condition can affect both the hard and soft palate, leading to a gap or split that can vary in size and shape. The incidence of cleft palate, either in isolation or combined with unilateral cleft lip, represents one of the most common birth anomalies, touching lives across all geographic regions and communities. Its cause is often attributed to a combination of genetic and environmental factors, though the exact cause remains unknown in many cases.
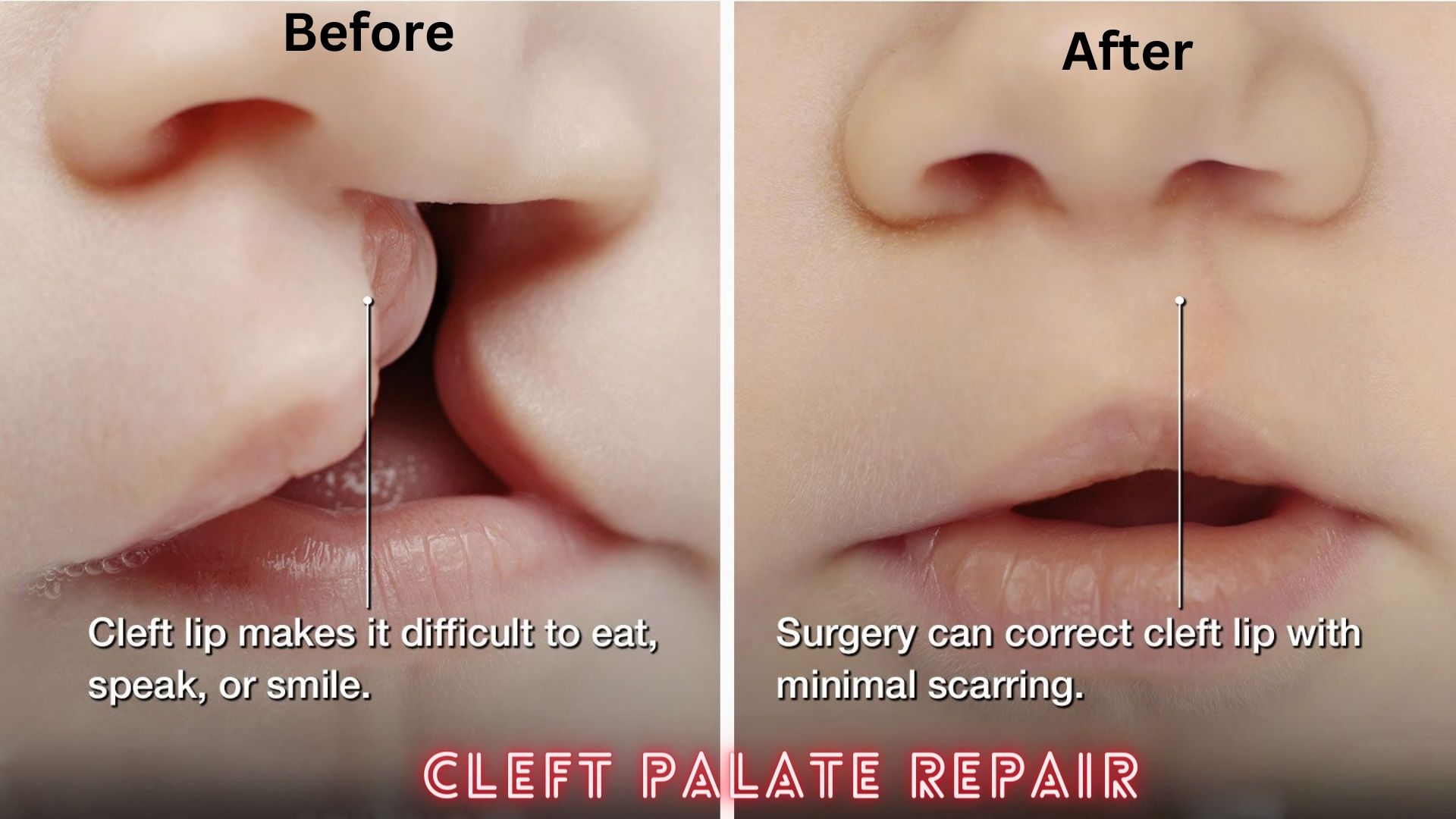
Children born with a cleft palate face various challenges. Beyond the apparent physical distinction, the condition can significantly impair essential functions such as eating, speaking, and hearing. Without proper treatment, it can also lead to recurrent ear infections, hearing loss, and difficulties with dental development and health.
The Importance of Addressing Cleft Palate Early
Early intervention for a cleft palate is crucial for several reasons. First, it significantly minimizes the risk of feeding, speech, hearing, and social integration complications. Early surgical repair, ideally performed within the first year of life, can dramatically improve outcomes in these areas. Moreover, addressing the condition early helps mitigate the emotional and psychological impact on the child and their family, fostering a more positive self-image as the child grows.
Intervening early also facilitates smoother integration into social environments, such as school, by reducing the likelihood of speech difficulties and boosting confidence. Furthermore, early repair can streamline the path for potential additional treatments, whether for speech, orthodontic needs, or secondary surgeries, by setting a solid foundation for further development and rehabilitation.
What is Cleft Palate Surgery?
Definition and Overview
Cleft palate surgery, medically known as palatoplasty, is a surgical procedure aimed at repairing the cleft lip and palate, restoring functionality, and achieving a more typical appearance of the mouth. The surgery involves the reconstruction of the palate by closing the gap or split, which not only improves the cosmetic appearance but, more importantly, enables the child to develop normal speech patterns, improves feeding and swallowing abilities, and reduces the risk of ear infections.
The specific technique used during surgery can vary depending on the type and extent of the cleft, the child’s age and health, and the surgeon’s expertise. The operation is typically carried out under general anesthesia and involves the careful realignment and stitching of the palate’s tissues and muscles to create a continuous, smooth surface.
The Goal of Cleft Palate Surgery
The primary goal of cleft palate surgery is to restore the functionality of the palate, allowing for normal speech development and adequate separation of the nasal and oral cavities to facilitate proper eating and breathing. This surgical intervention aims to:
- Improve Speech: By reconstructing the palate, the surgery aims to enable the child to develop normal speech patterns and reduce the likelihood of nasal-sounding speech.
- Enhance Feeding Ability: Closing the gap in the palate helps prevent food and liquids from entering the nasal cavity during eating, making feeding easier and more efficient.
- Reduce the Risk of Ear Infections and Hearing Loss: A properly repaired palate can help prevent fluid buildup in the middle ear, reducing the risk of recurrent ear infections and associated hearing problems.
- Support Dental and Facial Development: Early repair can facilitate better alignment and development of the teeth and jaws, contributing to a more typical facial structure as the child grows.
Preparing for Cleft Lip and Cleft Palate Repair
Initial Consultation and Evaluation
The journey towards cleft palate surgery begins with an initial consultation, where parents or caregivers and the patient (if old enough) meet with a cleft and craniofacial specialist. During this meeting, the surgeon will:
- Review Medical History: Discuss the patient’s medical history, previous surgeries, and current health status to understand the full scope of the patient’s needs.
- Conduct a Physical Examination: A thorough examination of the Cleft palate surgery is performed to assess its type and severity. This may involve looking at how the cleft affects the mouth, nose, and ears.
- Discuss Potential Treatment Options: Based on the initial assessment, the surgeon will outline the recommended surgical and non-surgical treatment options, providing a roadmap for care.
- Address Concerns and Expectations: Cleft palate surgery is a crucial time for parents and patients to voice their concerns, ask questions, and discuss their expectations with the surgeon.
Choosing the Right Surgeon
Selecting the right surgeon for cleft palate surgery is paramount. A surgeon’s expertise, experience, and approach to care can significantly impact the surgery’s outcomes. Here are key factors to consider:
- Specialization and Experience: Look for a surgeon who specializes in cleft and craniofacial surgery and has extensive experience performing cleft palate surgeries.
- Board Certification: Ensure the surgeon is board-certified in plastic surgery or a related field. This indicates that they have met rigorous standards in their specialty.
- Patient Reviews and Testimonials: Feedback from former patients can offer valuable perspectives on their experiences with the surgeon and the care team.
- Hospital Affiliations: Consider the quality of the facility where the surgery will be performed. A hospital or clinic specializing in pediatric and craniofacial conditions may offer higher care.
Types of Cleft Palate Surgery
Cleft palate surgery aims to repair the cleft, restore muscle function, and ensure the proper growth of the mouth and nasal structures. The primary types of surgery include:
Palatoplasty
Palatoplasty is the surgical procedure to repair the cleft palate, focusing on cosmetic and functional aspects. This surgery typically occurs when the child is between 6 and 12 months old. The goals of palatoplasty include closing the gap in the palate, realigning the muscles, and ensuring the palate can function correctly for speech.
Alveolar Bone Graft
An alveolar bone graft is usually performed when the child is between 8 and 12 years old, coinciding with the eruption of the permanent teeth. This procedure involves transplanting bone to the gap in the gum area, which supports the base of the nose and the teeth adjacent to the cleft and stabilizes the maxillary arch.
Secondary Surgeries and Revisions
Some patients may require secondary surgeries or revisions as they grow. These additional procedures can address aesthetic concerns, improve speech, or correct dental and orthodontic issues. Secondary surgeries are tailored to the individual’s needs and may include:
- Pharyngoplasty: A surgery to improve speech by adjusting the soft palate’s function.
- Rhinoplasty: Nose reshaping surgery to improve appearance and function.
- Orthognathic Surgery: Corrective jaw surgery to address significant jaw misalignments.
The Cleft Palate Surgery Procedure
Before the Surgery
Preparation for cleft palate surgery begins with comprehensive consultations with a multidisciplinary team, including a plastic surgeon, a pediatrician, and other specialists as needed. Patients undergo thorough evaluations, including physical examinations, imaging tests, and discussions about the expected outcomes and the procedure. Preparation also involves educating the family about the surgery, what to expect, and how to care for the child post-operatively. Instructions might include dietary restrictions, medication adjustments, and scheduling pre-operative visits. This phase is crucial for ensuring the child and their caregivers are fully prepared for the journey ahead. Also, please see my other post, Scabies In Human.
During the Surgery
Cleft palate surgery is typically performed under general anesthesia. The procedure’s length varies depending on the complexity of the cleft and the surgical technique used. The most common method, palatoplasty, involves reconstructing the palate to close the gap, realign the muscles, and ensure the mouth and nose are separated. This process often includes adjusting the tissue and muscles to enhance the palate’s function. The surgeon’s primary goals are to achieve a normal palate length, good speech outcomes, and minimal impact on facial growth.
After the Surgery: The Recovery Process
Post-operative care is vital for healing and includes pain management, dietary restrictions, and avoiding certain activities that could disrupt the surgical site. Initially, the child may require a liquid or soft diet and arm restraints to prevent touching the surgery area. Follow-up visits are essential to monitor healing, assess the need for further interventions, and begin any necessary speech therapy. Recovery times vary, but many children can return to normal activities within a few weeks with close monitoring and care from their healthcare team.
Risks and Complications of Plastic Surgery
Common Surgical Risks
As with any surgery, cleft palate repair carries risks such as bleeding, infection, and reactions to anesthesia. Specific to this surgery are risks of fistula development (small openings), which may require additional surgery to close, and challenges with feeding or breathing post-operatively. The surgical team takes great care to minimize these risks, but prompt attention to any signs of complications is crucial.
Long-term Complications and Management
Some children may face long-term challenges, such as speech, hearing, and dental issues, necessitating ongoing care. Speech therapy is often required to address articulation problems. Regular hearing check-ups and treatments for fluid buildup can prevent hearing loss. Orthodontic treatments may be needed to address teeth alignment and jaw growth issues. A proactive, multidisciplinary approach ensures these complications are managed effectively, allowing the child to thrive.
- Regular monitoring and check-ups to detect and address complications early.
- Lifestyle modifications, including diet and exercise, support overall health and mitigate risk factors.
- Medication adherence to manage symptoms and slow the progression of the condition.
- Psychological support and counseling to help cope with the emotional and mental health challenges of living with a chronic condition.
Life After Cleft Lip Repair and Surgery
Speech Therapy and Rehabilitation
Speech therapy is a cornerstone of post-operative care for children undergoing cleft palate surgery. A speech-language pathologist specializes in helping children improve their speech articulation, overcome language challenges, and develop effective communication skills. Therapy may begin shortly after surgery and continue for several years, tailored to the child’s needs and progress.
Psychological and Social Aspects
The psychological and social implications of living with a cleft palate and undergoing surgery cannot be underestimated. Children may face self-esteem, social interactions, and emotional well-being challenges. Support from psychologists, counselors, and peer support groups can be invaluable. Education and advocacy are key to promoting understanding and inclusion, helping children and their families navigate these challenges, and celebrating their strengths and achievements.
- Enhanced Self-Esteem: Surgery can significantly improve physical appearance, boosting self-confidence and social interactions.
- Speech Improvement: Correcting the cleft palate often leads to better speech outcomes, reduced social stigma, and improved communication skills.
- Social Integration: Successful surgery can facilitate easier integration into social settings, reducing isolation and enhancing peer relationships.
Frequently Asked Questions (FAQs) about Cleft Palate Surgery
Q1. What is the best age for cleft palate surgery?
Cleft palate surgery is typically recommended for children between 9 and 18 months old. This timing helps ensure optimal healing and reduces the impact on speech development.
Q2. Can a cleft palate recur after surgery?
While the physical cleft cannot recur after surgery, issues such as fistulas (small openings) may develop and require additional treatment. Ongoing assessments are important for addressing any complications early.
Q3. How long does recovery from cleft palate surgery take?
Initial healing from surgery often takes about 2 to 3 weeks, but complete recovery, including the resolution of swelling and full healing of the palate, can take several months. Follow-up care is essential during this period.
Q4. What are the success rates of cleft palate surgery?
Success rates are high, with most children achieving significant speech, feeding, and appearance improvements. However, outcomes can vary based on the extent of the cleft and individual health factors.