Meningitis B
What is Meningitis B?
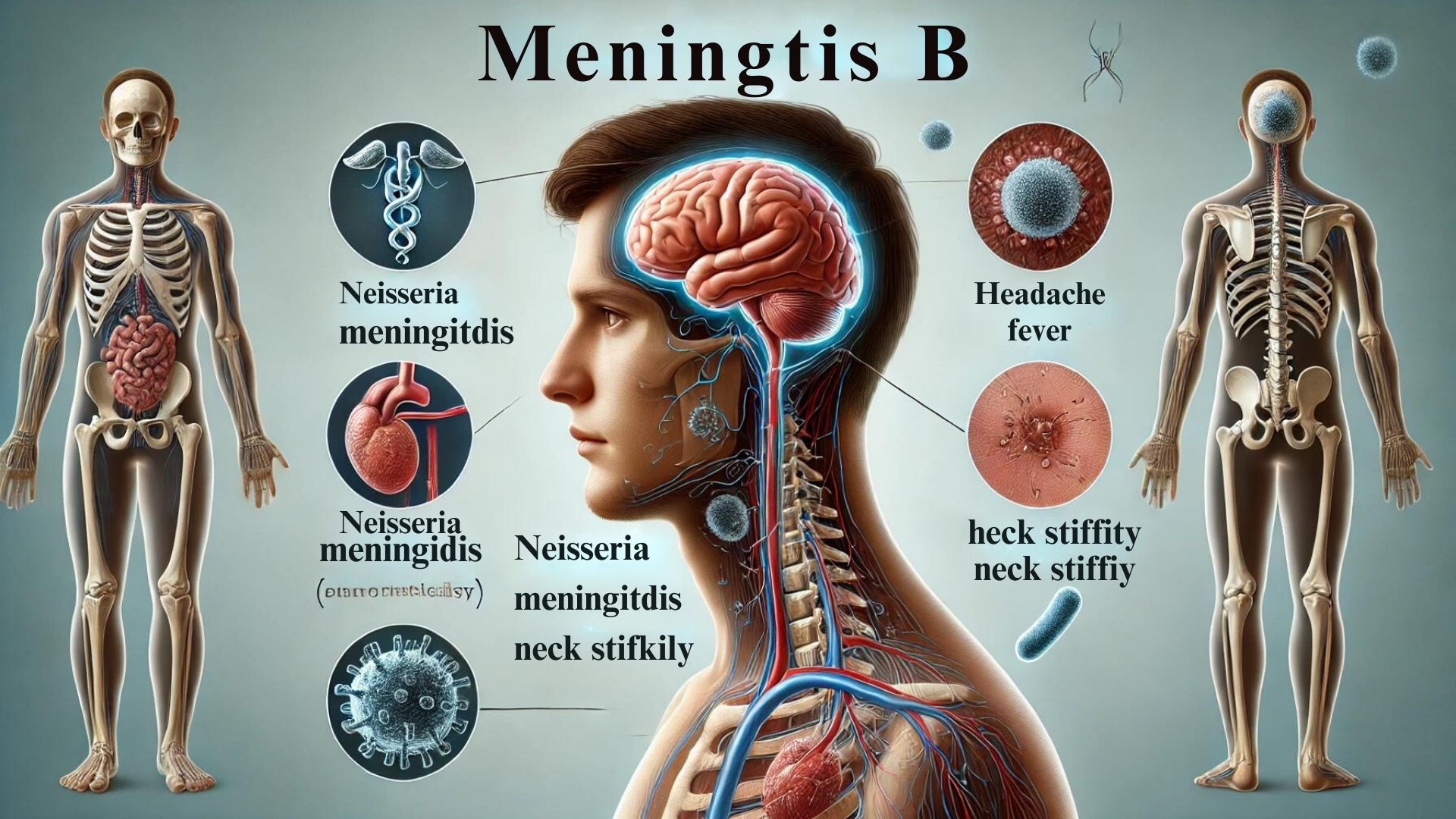
Meningitis B is a severe infection caused by the bacterium Neisseria meningitidis serogroup B. This form of meningitis primarily affects the protective membranes covering the brain and spinal cord, known as the meninges. It can lead to significant health complications and is potentially life-threatening if not treated promptly. Meningitis B is particularly notable for its ability to cause rapid onset of symptoms and its prevalence among certain age groups, particularly infants, teens, and young adults.
Causes of Meningitis B
The disease is caused by the group B strain of the bacterium Neisseria meningitidis. It spreads through respiratory and throat secretions—commonly transmitted by coughing, kissing, or sharing utensils with an infected person. Outbreaks are frequent in closed or semi-closed communities, including schools, college dormitories, and military barracks. Understanding the transmission methods is crucial for prevention and control.
Importance of Awareness
Raising awareness about Meningitis B is critical because early recognition and treatment significantly improve prognosis. Public education campaigns can inform people about vaccination, which is an effective prevention measure. Awareness also helps in recognizing the signs and symptoms early, allowing for quicker medical intervention, which can be life-saving.
Symptoms of Meningitis B
Early Symptoms
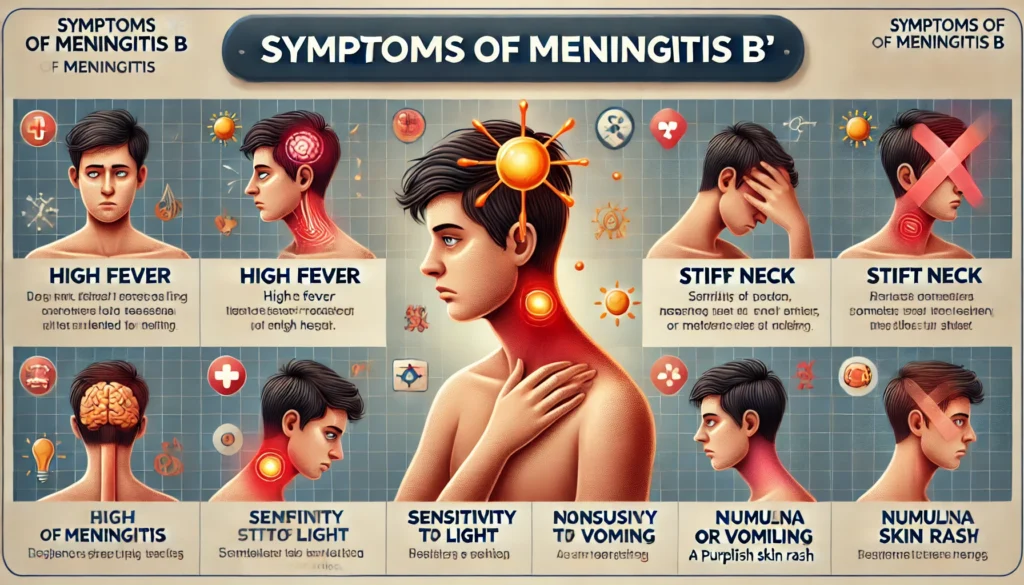
Meningitis B symptoms can initially resemble those of the flu, which often leads to initial misdiagnosis. Early symptoms include:
- Fever
- Headache
- Fatigue or drowsiness
- Stiff neck
- Irritability
- Increased sensitivity to light
Recognizing these early symptoms is vital as they can quickly progress to more severe complications.
Severe Symptoms
As the infection progresses, more severe symptoms may develop, including:
- Severe headache that doesn’t go away
- Nausea and vomiting
- Confusion and difficulty concentrating
- Seizures
- Sleepiness or difficulty waking up
- Skin rash (purple or red spots that don’t fade under pressure)
These symptoms indicate an advanced infection requiring immediate medical attention.
When to Seek Medical Help
Medical help should be sought immediately if any signs or symptoms of Meningitis B are observed, especially if they rapidly worsen. The condition is a medical emergency, and delaying treatment can result in severe complications or death. Prompt treatment with antibiotics and supportive care in a hospital setting can greatly increase the chances of a full recovery.
Risk Factors and Vulnerable Populations
Age Groups at Risk
Meningitis B can affect individuals of any age, but certain age groups are at higher risk. Infants and young children under five years old are particularly susceptible due to their developing immune systems. Adolescents and young adults, especially those living in communal environments like college dormitories or military barracks, also face a higher risk. Understanding these age-specific vulnerabilities can help target preventive measures more effectively.
Lifestyle Factors
Certain lifestyle choices and behaviors can increase the risk of contracting Meningitis B. Close and prolonged contact with many people, such as in bars, dormitories, or through frequent travel, can elevate exposure to the bacterium. Additionally, individuals who smoke or are exposed to secondhand smoke may have an increased risk, as smoking can damage the mucous membranes, making it easier for the bacteria to invade the body.
Underlying Health Conditions
People with compromised immune systems, whether due to medical treatments like chemotherapy, diseases such as HIV/AIDS, or genetic disorders affecting immunity, are more susceptible to Meningitis B. Similarly, those with persistent viral infections or chronic diseases that weaken the body’s defenses are at elevated risk. These individuals must take preventive measures and be vigilant about possible symptoms.
Transmission of Meningitis B
How Meningitis B Spreads
Meningitis B is primarily spread through respiratory droplets when an infected person coughs or sneezes. The bacteria can also be transmitted through close personal contact, such as kissing or sharing eating utensils, lip balms, or cigarettes. Understanding these modes of transmission can help in adopting effective preventive strategies.
Common Environments for Transmission
Outbreaks of Meningitis B are often associated with places where large groups of people gather close together. Schools, college dormitories, military barracks, and childcare facilities are common environments for the spread of the disease. In these settings, the close quarters facilitate the easy transfer of respiratory droplets from one person to another, increasing the risk of infection.
Preventing Spread in Community Settings
Preventing the spread of Meningitis B in community settings involves several strategies. Vaccination is the most effective preventive measure. Ensuring that people, especially those in high-risk groups, are vaccinated can significantly reduce the incidence of the disease. Additionally, maintaining good hygiene practices such as regular hand washing, covering the mouth and nose with a tissue or sleeve when coughing or sneezing, and not sharing personal items can help prevent the spread of bacteria. In outbreak settings, health authorities might recommend prophylactic antibiotics to close contacts of a diagnosed case to prevent further spread.
Diagnosis of Meningitis B
Diagnostic Tests
The diagnosis of Meningitis B begins with several key tests that help identify the presence of Neisseria meningitidis bacteria. Initially, blood tests are performed to check for signs of infection, such as elevated white blood cell counts. Blood cultures may also be used to try to grow the bacteria from a sample, confirming the diagnosis.
Another crucial diagnostic tool is imaging tests like MRI or CT scans. These are not used to detect the bacteria directly but to view the brain and spinal cord for signs of swelling or inflammation, which are indicative of meningitis.
-
- Blood Tests
- Polymerase Chain Reaction (PCR) Tests
- Culture Test
Medical History and Physical Examination
A thorough medical history and physical examination are vital components in diagnosing Meningitis B. During the history-taking, doctors inquire about symptoms, vaccination history, and any recent exposures to potential sources of infection. The physical exam will include checking for typical signs of meningitis, such as neck stiffness, fever, and altered mental state. Other signs that might be assessed include the presence of a rash, which can be characteristic of meningococcal meningitis.
The Role of Lumbar Puncture
Lumbar puncture, or spinal tap, is the definitive test for diagnosing Meningitis B. In this procedure, a needle is inserted into the lower part of the spinal canal to collect cerebrospinal fluid (CSF), which surrounds the brain and spinal cord. The CSF is then analyzed for markers of infection, including elevated white blood cell count, increased protein levels, and, most importantly, the presence of bacteria through Gram stain and culture. This test not only confirms the diagnosis but also helps in determining the specific type of bacteria responsible, guiding treatment choices.
Treatment Options

Immediate Treatments
Immediate treatment for Meningitis B is critical and focuses on eradicating the infection and managing symptoms. Antibiotic therapy must start as soon as Meningitis B is suspected, even before diagnosis is confirmed, due to the rapid progression of the disease. The choice of antibiotics may later be adjusted based on the results of the CSF culture. Supportive care is also crucial and includes fluid management, stabilization of blood pressure, and, in severe cases, measures to reduce brain swelling and prevent seizures.
-
- Antibiotics
- Supportive Care
Long-term Care Needs
Survivors of Meningitis B may require long-term care due to potential complications like hearing loss, cognitive deficits, or motor function impairments. Rehabilitation services may include physical therapy, occupational therapy, and speech therapy, depending on the specific needs of the individual. Regular follow-up appointments are essential to monitor recovery and manage any ongoing health issues.
-
- Rehabilitation: Physical, occupational, and speech therapy may be necessary depending on the severity of the complications experienced.
- Monitoring: Regular follow-ups to monitor neurological health, hearing, and overall physical recovery are essential.
Innovations in Treatment
Recent advancements in the treatment of Meningitis B include the development of more effective vaccines, which have significantly reduced the incidence of the disease. Research is ongoing into new antibiotic therapies and methods to reduce the inflammatory damage caused by the infection. Additionally, there’s growing interest in the use of adjuvant treatments that can modulate the immune response to help reduce the severity of the symptoms and prevent complications.
- Vaccine Development
- Advanced Antibiotic Therapies
Vaccinations and Prevention

Available Vaccines
Meningococcal disease, which includes Meningitis B, can be prevented through vaccination. The primary vaccines available for Meningitis B are Bexsero and Trumenba. These vaccines are specifically targeted against the serogroup B meningococcal bacteria. They work by triggering the body’s immune system to produce antibodies against the bacterium, thus protecting against the disease.
Vaccination Schedules
For maximum effectiveness, the Centers for Disease Control and Prevention (CDC) recommends different vaccination schedules based on age and risk factors. For adolescents, the typical recommendation is for two doses of a serogroup B meningococcal vaccine. The first dose is usually administered at age 16, with a booster dose given at age 18. For those at increased risk due to certain medical conditions or because of a serogroup B meningococcal disease outbreak in their community, vaccination might be recommended earlier and with additional doses.
Effectiveness and Safety
Clinical trials and post-marketing surveillance have shown that vaccines like Bexsero and Trumenba are effective in preventing Meningitis B among individuals who receive the vaccine. The vaccines are generally safe, with the most common side effects being mild including soreness at the injection site, fatigue, and fever. Severe reactions are rare, and the benefits of vaccination in preventing Meningitis B far outweigh the potential risks.
Complications and Consequences
Short-term Complications
Meningitis B can lead to severe short-term complications if not treated promptly. These can include septicemia (blood poisoning), severe brain damage, and hearing loss. The inflammation caused by the infection can result in symptoms like severe headache, fever, and neck stiffness, and can escalate quickly to more severe conditions such as seizures and coma.
Long-term Health Effects
Survivors of Meningitis B can suffer from long-term effects, which may include physical and neurological damage. These effects can be life-altering and include hearing loss, cognitive deficits, memory difficulties, and motor function impairments. In some cases, limb amputation might be necessary due to the effects of septicemia associated with the infection.
Psychological Impact
The psychological impact of Meningitis B, both on survivors and their families, can be profound. Survivors may experience emotional challenges such as anxiety, depression, and post-traumatic stress disorder (PTSD). Additionally, the fear of recurrence and the stress of coping with any permanent disabilities can significantly affect their quality of life. Support from mental health professionals, along with community and family support, is crucial in helping individuals recover not just physically but also emotionally and psychologically.
Global Impact and Statistics
Prevalence Worldwide
Meningitis B is a global health concern with cases reported on every continent. The incidence of Meningitis B varies significantly between countries and regions, influenced by factors such as vaccination policies, healthcare access, and public health practices. In industrialized nations, widespread vaccination has significantly reduced the prevalence, but in low-income countries, the disease remains a major threat, especially among infants and young children.
Recent Outbreaks
Recent outbreaks of Meningitis B have highlighted the disease’s unpredictable nature and the importance of vigilance and preparedness. For example, several university campuses in the United States have experienced outbreaks over the past decade, leading to renewed efforts in booster vaccination campaigns. These incidents remind us that Meningitis B can occur in any setting where individuals are in close contact.
Efforts in Eradication
Global efforts to eradicate Meningitis B are primarily focused on vaccination and improving healthcare responses during outbreaks. The World Health Organization (WHO), in collaboration with various governments and NGOs, has launched initiatives to increase vaccine coverage in underdeveloped regions. Additionally, advancements in vaccine research aim to develop more effective and longer-lasting vaccines, which are crucial for eradication efforts.
Living with Meningitis B
Lifestyle Adjustments
Surviving Meningitis B can mean significant lifestyle adjustments, particularly for those who experience long-term effects such as hearing loss, cognitive impairments, or motor function deficits. Individuals may need to adapt their living environments, pursue rehabilitation, and use assistive devices. Adapting to these changes is critical for improving quality of life and achieving independence.
Support Networks
Support networks play a crucial role in the recovery and adjustment process for survivors of Meningitis B and their families. These networks can include healthcare professionals, peer support groups, and non-profit organizations dedicated to meningitis. Emotional and practical support from these networks helps individuals navigate the complexities of recovery and adaptation.
Future Outlook
The future outlook for those living with Meningitis B is improving with advances in medical treatment and rehabilitative care. Research into neurological recovery and support systems continues to evolve, offering hope for better recovery outcomes. Furthermore, ongoing improvements in vaccine formulations and delivery are expected to reduce the incidence of the disease, thereby minimizing the long-term impacts on individuals and communities.

Conclusion
Frequently Asked Questions (FAQs) about Meningitis B
What causes Meningitis B?
Meningitis B is caused by the bacterium Neisseria meningitidis, specifically the B strain. It affects the membranes surrounding the brain and spinal cord, leading to severe infection.
How is Meningitis B transmitted?
The disease spreads through respiratory droplets or throat secretions from infected individuals. Common methods of transmission include coughing, sneezing, kissing, or sharing utensils and drinkware.
Who is most at risk for Meningitis B?
While anyone can contract Meningitis B, certain groups are at higher risk, including infants, adolescents, and young adults, particularly those living in close quarters like dormitories or military barracks.
What are the symptoms of Meningitis B?
Symptoms often include fever, headache, stiff neck, nausea, vomiting, increased sensitivity to light, and confusion. These symptoms can develop rapidly and require immediate medical attention.
Can Meningitis B be prevented?
Yes, vaccination is the most effective way to prevent Meningitis B. There are vaccines specifically designed to protect against Neisseria meningitidis Group B, recommended for people in high-risk groups or during outbreaks.